Can Dermarolling Relieve Periorbital Melanosis? Is Dermarolling Therapy a Good Treatment Option?
Do you have periorbital melanosis or presence of dark circles around the eyes? It is a commonly encountered condition. It is also popularly known in other terms such as periocular hyperpigmentation, dark circkes, infraorbital darkening, idiopathic cutaneous hyperchromia or infraorbital discoloration.
Most dermatologists would agree that they commonly encountered this condition in their clinical practice.
People who have dark circles around the eyes complained of cosmetic concerns. Whenever their taking some pictures, they feel uncomfortable because of cosmetic reasons. Of course, it is not good to look at a person with dark circles because they either look so tired or it may seem that they lack good night sleep.
Periorbital melanosis can affect a person’s emotional well-being. It may also influence their quality of life.
Why does periorbital melanosis occur?
Although, it is a commonly encountered condition, there is little scientific data that would provide a thorough clinical profile on why this condition occurs. There are many possible factors why periorbital hyperpigmentation occurs.
It could be due to heredity or genetic factors, post inflammatory hyperpigmentation secondary to allergic or contact dermatitis, excessive pigmentation, excessive vascularity, tear trough associated with aging, and or shadowing due to laxity of the skin.
The good news is – there are a number of treatment options available to treat dark circles. The available alternatives include:
- Topical depigmenting agents such as topical retinoic acid, azelaic acid, kojic acid, and hydroquinone
- Physical therapies like chemical peels, laser therapy, surgical corrections and microneedling or dermarolling therapy
The goal of treatment is to determine and treat the main cause of hyperpigmentation and its contributory factors.
Who are the most commonly affected with this condition?
There is very few data that would present the incidence (new cases) and prevalence of dark circles because of its lack or reasonable etiological explanation and its transitory nature. It was found out in a recent study that this condition is common among 16 to 25 years old. It is common among women than men.
Majority of the affected population are housewives according to an Indian study.
How does periorbital melanosis generally look like?
Clinically a person with periorbital melanosis has brownish-black to dark-colored pigmentation surrounding the eyelids. A person with dark circles gives a tired look appearance. Doctors may based their diagnosis by clinical examination.
Dark circles are different from dark eyelid skin with shadowing due to a tear trough. Manual stretching of a person’s lower lid can differentiate between shadowing effect and true pigmentation. A true pigmentation retains its appearance even after stretching while shadowing effect resolves or improves entirely.
The increase in violaceous discoloration due to manual stretching of the lower eyelid can be due to hypervascularity of the lower eyelid or due to thin eyelid skin. Doctors may use different examination to differentiate pigmentations from one another. An ultrasound may be used to differentiate periorbital puffiness from vascular origin.
How genetic factors contribute to Periorbital hyperpigmentation?
The darkening of the circles around the eyes can be due to genetic factors. Families who have pigmentation around the periorbital area have several members of the family having the same condition. Some can be mildly affected while others can be severely affected.
Many of the family members recognized the dark circles early in childhood. They also claimed that the pigmentation increases with age. They also stated that stress can trigger intense pigmentary changes while good health and rest seems to produce lessening of the discoloration. There is even familial case where the affected family members run through six generations.
Causes of periorbital melanosis
Aside from genetic influence periorbital melanosis can also be caused by several other factors including:
Presence of melanocytes in the dermis
Dermal melanocytosis is the presence of melanocytes in the dermis. It is recognizable by its blue-grey or distinctive grey appearance. Dermal melanocytosis causing periocular hyperpigmentation can be caused by congenital or acquired factors.
Periorbital hyperpigmentation is usually diagnosed if it is located infraorbitally. It appears as blue-black patches or mottled brown-grey which may involve the infraorbital area.
Postinflammatory hyperpigmentation
Excessive pigmentation are caused by postinflammatory hyperpigmentation secondary to allergic or atopic contact dermatitis and other dermatological conditions such as lichen planus pigmentosus and or drug induced. It can be caused by fixed drug eruptions and erythema dyschromium perstans.
The hyperpigmentation in the periorbital area can be caused by scratching and rubbing the skin around the eyes because of the accumulation of fluid due to atopic dermatitis or allergy and or allergic contact dermatitis.
Thin skin covering the eye muscles
Superficial location of vasculature and having thin skin covering the orbicularis oculi or eye muscles is another cause of periorbital hyperpigmentation. This condition involves the entire lower eyelid. It has violaceous appearance because of prominent blood vessels covered by a thin layer of the skin.
It is more in the inner aspect of the eyelid usually accentuated during menstrual period. When the lower eyelid is stretched manually, the dark areas spreads without significant lightening or blanching and results to a deepening of violaceous color. This could be used as diagnostic test to determine vascularity.
Tear trough depression
Tear troughs are anatomical location that become depressed as one grows older. It is center over the inferior to medial orbital rim. It is classified as age-related change. It occurs because of thinning of overlying skin of the orbital rim ligaments or loss of subcutaneous fats. The combination of hollowness and overlying pseudoherniation of the infraorbital fat accentuate the shadowing in the tear through that causes dark circles depending on the condition of the lighting.
Periorbital edema
The eyelid area has spongy property which leads to fluid accumulation due to local and systemic causes. The presence of edema appears after eating salty meals or it is worse in the morning. The presence of edema may influence the presence of periorbital hyperpigmentation depending on the extension and variability.
Ocular hypotensive drugs
Latanoprost and bimatropost are prostaglandin analogues which are used as ocular hypotensive eye drops in patients with glaucoma. It may also cause periorbital hyperpigmentation if used frequently around 3 to 6 months of therapy. Complete reversal of hyperpigmentation occurs after discontinuation of the treatment.
Environmental causes
Ultraviolet radiation and other lifestyle factors may contribute to dark circles around the eyes. Ā Other factors such as stress, lack of sleep, smoking, and alcohol overuse may aggravate the skin’s condition.
The role of dermarolling therapy in treating periorbital hyperpigmentation
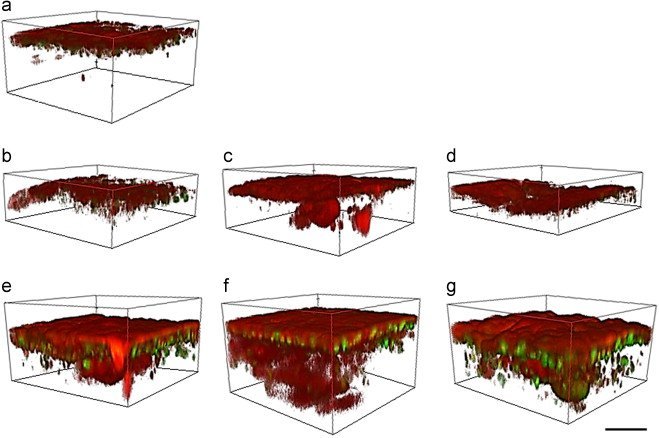
There are a number of studies that have been proposed as to the role and potential of microneedling or dermarolling as an alternative treatment to conventional therapy for pigmentation disorders affecting dark skin types including vitiligo, melasma and periorbital hyperpigmentation.
The enhanced drug absorption due to transdermal approach seen with microneedling has achieved better results as compared with skin lightening agents alone in treating melasma. Microneedling is a good combination therapy that provides favourable results when combined with daily sunscreen use.
Bibliography
Christopher Iriarte,1 Olabola Awosika,2 Monica Rengifo-Pardo,1,2 and Alison Ehrlich1,2. (2017). Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. , 289-298.
Rashmi Sarkar, MD, MNAMS, Rashmi Ranjan, MD, Shilpa Garg, DNB, Vijay K. Garg, MD, MNAMS, Sidharth Sonthalia, MD, DNB, and Shivani Bansal, MD, DNB. (2016). Periorbital Hyperpigmentation: A Comprehensive Review. J Clin Aesthet Dermatol. , 49-55.







Please add your thoughts
Leave a Reply
Want to join the discussion?Feel free to contribute!